What is post-concussion syndrome?
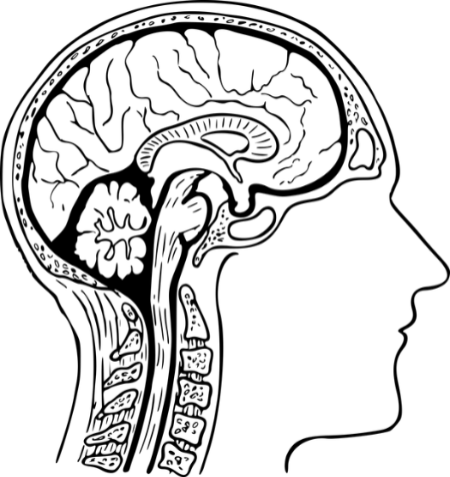
Post-concussion syndrome (PCS) occurs when symptoms resulting from a concussion, also known as a mild traumatic brain injury (mTBI), persist beyond the expected timeframe of recovery.
- While there is disagreement among the literature as to the exact duration of symptoms necessary for this diagnosis, one month is the most common timeframe cited.
- The most common post-concussive symptom is headache, followed by dizziness, which is more often a sense of disequilibrium and imbalance than of true vertigo.
- Initial injury severity does not appear to correlate with the likelihood of developing post-concussion syndrome. However, a history of past concussions does appear to correlate with the likelihood of PCS development.
A study comparing children and adolescents with sport-related concussions who had short recovery times (30 days or less) to those who developed post-concussion syndrome, found that PCS was more likely to occur in:
- Patients who reported amnesia at the time of concussion
- Patients diagnosed with vestibulo-ocular dysfunction (double the average recovery time as those without VOD, and 4X higher odds of developing PCS) Patients with higher PCSS scores (concussion severity indicator)
- Other Risk Factors identified in the literature are age, gender (female), previous concussion, previous migraine, loss of consciousness at the time of injury.
- Studies suggest that 21-59% of patients age 18 and younger who experience a concussion will develop persistent symptoms lasting longer than one month.
Post-concussion dysfunction (PCD), is differentiated into physiological PCD, vestibulo-ocular PCD and Cervicogenic PCD.
- Symptoms of Physiological PCD may include:
- Headache that worsens with physical and cognitive exertion, nausea, vomiting, sensitivity to light and sound, dizziness, fatigue, poor concentration, and slow speech
- Symptoms of Vestibulo-ocular dysfunction (VOD) may include:
- Vertigo, dizziness, motion sensitivity, postural/gait imbalances, blurred vision, gaze instability, disequilibrium, or diplopia
- Symptoms of Cervicogenic PCD may include:
- Painful and/or stiff neck, limited ROM, occipital headache triggered by neck movements, dizziness, or postural issues
Assessment of Post-Concussion Syndrome
- Buffalo Treadmill Testing:
- Can be used to differentiate between alteration of brain metabolism (physiological PCD) and neural subsystem involvement (vestibulo-ocular PCD or cervicogenic PCD).
- Patients may be considered to be recovered when they have minimal to no symptoms at rest and attain maximal exertion without worsening of symptoms. At this point, they can safely return to physical activities. If patients still have symptoms 3 weeks after the injury and experience symptoms during the treadmill test, they may have physiological PCD.
- If patients still have symptoms at rest three weeks after their injury, but they don’t experience any symptoms during the treadmill test, an additional examination is necessary to identify whether their symptoms could be due to vestibulo-ocular PCD or cervicogenic PCD.
- Vestibulo-ocular Clinical Exam:
- Involves standardized techniques such as the evaluation of extra-ocular movement, smooth pursuits, near-point convergence (NPC), horizontal and vertical saccades, and the vestibulo-ocular reflex (VOR). In addition to vestibular and visual dysfunction, other potential causes of persistent dizziness can include cervical spine dysfunction, post-traumatic migraine, and autonomic dysfunction.
- Helpful Outcome Measures: Dizziness Handicap Inventory (DHI), Activities-specific Balance Confidence Scale (ABC), PostConcussion Symptoms Scale (PCSS), and Visual Vertigo Scale.
If you have experienced any brain trauma, we have Concussion certified physiotherapists here at Pivotal Physiotherapy that will be able to perform an assessment and provide you with treatment to get you back to your everyday life.
Treatment for Post-Concussion Syndrome
- Physiological PCD:
- Graded, sub-symptom exertional exercise.
- Energy conservation/pacing strategies for ADL’s
- Gradual reintroduction to stimulating or challenging environments/tasks
- Referral for medical management as appropriate
- Vestibuloocular Dysfunction:
- When symptoms of concussion such as dizziness, vertigo, and imbalance fail to recover spontaneously, vestibular rehabilitation can be used effectively to aid in the normalization of a patient’s vestibular responses. Vestibular rehab involves the use of specific exercises that aim to alleviate symptoms of vestibular dysfunction, as well as improve balance and the overall function of the patient.
- Dynamic gaze stability:
- The ability to maintain focus while the head is in motion is controlled primarily by the vestibular ocular reflex (VOR), cervical ocular reflex (COR), smooth pursuit, and optokinetic responses.
- Exercise: The patient focuses on a target which is stationary at first (VORx1), then moving (VORx2) while the head is rotated. Progressions can include increasing speed, and introducing coordination tasks.
- Static and dynamic balance controlled through combined input from the visual, vestibular, and somatosensory systems – can often become impaired following a concussion. Thorough testing needs to be performed to assess all three contributing systems and how they are functioning together for a particular patient. Exercise components:
- Beginning with basic environments and progressing to more complex ones
- Eyes open versus eyes closed
- Head turns and tilts
- Stable versus unstable surfaces
- Cervicogenic PCD:
- Treat the affected musculoskeletal structures as appropriate
- Treatment follows typical whiplash-associated disorder protocols including neck and shoulder stretching, strengthening, and proprioceptive exercises.
- Consideration may also be given to temporal-mandibular joint dysfunction
Prognosis and Typical Rehab Timelines
Extremely variable based on the cause of the patient’s PCD. Symptoms nearly always resolve, although depending on confounding factors at play as well as the extent of brain injury sustained, symptoms can last many months or even over a year in severe cases.
References
- Aubry M, Cantu R, Dvorak J, Graf-Baumann T, Johnston K, Kelly J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001. Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002 Feb;36(1):6-10.
- Dannenbaum E, Chilingaryan G et al. Visual vertigo analogue scale: an assessment questionnaire for visual vertigo. J Vestib Res. 2011. 21(3): 153-159.
- Ellis MJ, Cordingley D, Vis S, Reimer K, Leiter J, Russell K. Vestibulo-ocular dysfunction in pediatric sports-related concussion. J Neurosurg Pediatr. 2015 https://pubmed.ncbi.nlm.nih.gov/26031619/ [cited 2016 May 31]; 16:248-255.
- Ellis MJ, Leddy JJ, Willer B. Physiological, Vestibulo-ocular and cervicogenic post-concussion disorders: An evidence-based classification system with directions for treatment [Internet]. Taylor & Francis. [cited 2023Apr16].
- Gurley JM, Hujsak BD, Kelly JL. Vestibular rehabilitation following mild traumatic brain injury. NeuroRehabilitation. 2013 [cited 2016 May 31]; 32:519-528.
- Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, Kutcher JS, Pana A, Putukian M, Roberts WO. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013 Jan;47(1):15-26. doi: 10.1136/bjsports-2012-091941. Erratum in: Br J Sports Med. 2013 Feb;47(3):184. PMID: 23243113.
- Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolanryngol Head Neck Surg. 1990;116:424–427.
- Mullally, William J., MD. Concussion. The American journal of medicine. 2017;130(8):885–92.
- Powell LE and Myers AM. (1995). “The Activities-specific Balance Confidence (ABC) Scale.” Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 50A(1): M28-34.
- Tator CH, Davis HS, Dufort PA, Tartaglia MC, Davis KD, Ebraheem A, Hiploylee C. Postconcussion syndrome: demographics and predictors in 221 patients. J Neurosurg. 2016 Nov;125(5):1206-1216. doi:10.3171/2015.6.JNS15664. Epub 2016 Feb 26. PMID: 26918481.
