What is Stress Urinary Incontinence (SUI)?
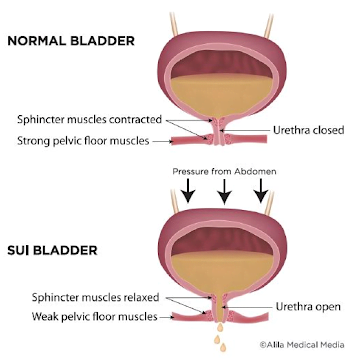
Stress Urinary Incontinence (SUI) is an involuntary leakage of urine during effortful movements, physical activity, or movements of the body that can cause pressure in the abdomen.1,2 This common and treatable condition may occur due to damage, weakness, or loss of motor control of the pelvic floor.
Common symptoms of SUI
These mainly include a loss urine with movements such as 2,4:
- Coughing
- Sneezing
- Laughing
- Running
- Jumping
- Lifting heavy objects
What is the Pelvic Floor?
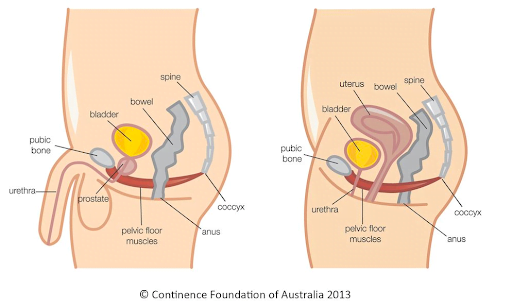
Think of the pelvic floor as a sling of muscles that attach from the pubic bone, at the front of your pelvis and extend to your tailbone, and connect horizontally to the bottom of each pelvic bone.5,6 This sling of muscles plays a large role in helping our bodies function.
The Pelvic Floor
- Provides support to the bladder and bowels in the abdomen
- Assists with bowel and bladder function
- Supports the uterus in females
- Plays a role in the sexual function of all individuals
- Works in unison with abdominal and back muscles to help stabilize and support the spine during movement
Who Experiences SUI?
SUI can effect people of all ages for a variety of reasons. For individuals with female reproductive anatomy, SUI can present during pregnancy, post-partum, and post-menopause.4 In this case, decreased strength and control of the pelvic floor can occur due to hormonal and structural changes during pregnancy, childbirth trauma, age-related hormone changes, and a history of surgery or prolapse in the pelvic floor region.1 SUI can also occur in individuals with male reproductive organs for reasons that may include, but are not limited to, an enlarged prostate gland, surgical removal of the prostate gland, or any other surgeries or medical treatment in the pelvic floor region.4
Pelvic Health Physiotherapy for Stress Urinary Incontinence
There can be a negative stigma associated with seeking help for SUI and other pelvic health concerns. For example, it is common for individuals to avoid participating in the physical activities they love due to the constant fear of having an accident.1,2,4 Many people also believe that incontinence is a normal part of aging, and that they have to live with the symptoms for the rest of their lives; but this is actually false!4
There are techniques and exercises that can be used to decrease and/or resolve problems of stress urinary incontinence.1,3 These all fall under the umbrella term of “Pelvic Health Physiotherapy (PFPT).
Several studies have shown that Pelvic floor Physiotherapy should be used as a first-line conservative strategy to treat stress urinary incontinence.3 It has been proven that PFPT has a positive effect on quality of life, improving symptoms, decreasing leakage episodes, and can even cure cases of urinary incontinence.3
What to expect
Pelvic floor physiotherapy treatment is highly individualized to each patient.
- Your assessment is performed by a Pelvic Health Physiotherapist in a private room to ensure your comfort.
- Every patient is different so the first assessment is a great time to sit down with your physiotherapist and determine your goals in order for them to create the right plan to help you achieve them.
- Like all physiotherapy sessions, your physiotherapist will educate you on your condition, and teach you exercises that you can complete when you leave the session.
Our pelvic health physiotherapists are extremely professional, knowledgeable and compassionate. If you are experiencing stress incontinence, don’t hesitate to reach out and book your appointment with them today!
By Shelby Shapka, MScPT Student
References
- Radziminska, A., Straczynska, A., Weber-Rajek, M., Styczynska, H., Strojek, K., & Piekorz, Z. (2018). The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: a systematic literature review. Clinical Interventions In Aging, 13, 957–965. https://doi-org.login.ezproxy.library.ualberta.ca/10.2147/CIA.S160057
- Lawson, S., & Sacks, A. (2018). Pelvic Floor Physical Therapy and Women’s Health Promotion. Journal Of Midwifery & Womens Health, 63(4), 410–417. https://doi-org.login.ezproxy.library.ualberta.ca/10.1111/jmwh.12736
- Dumoulin, C., Cacciari, L. P., & Hay-Smith, E. J. C. (2018). Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Of Systematic Reviews, 10, CD005654. https://doi-org.login.ezproxy.library.ualberta.ca/10.1002/14651858.CD005654.pub4
- The Canadian Continence Foundation. (n.d.). FAQ’s: Urinary Incontinence. Retrieved October 22, 2022 from
https://www.canadiancontinence.ca/EN/frequently-asked-questions.php#:~:text=As%20many%20as%203.3%20million,their%20doctor%20about%20their%20symptoms. - Continence Foundation of Australia. (2022, August 3). Continence Health: Pelvic Floor Muscles. Retrieved October 2, 2022 from https://www.continence.org.au/about-continence/continence-health/pelvic-floor
- Physiopedia. (n.d.). Pelvic Floor Dysfunction. Retrieved October 2, 2022 from https://www.physio-pedia.com/Pelvic_Floor_Dysfunction
