Since I neglected to introduce myself in my first blog post, I want to take this opportunity to provide some background and explain why I have ventured to Pivotal Physiotherapy. My name is Nicole Geier, some of you may know me as Nickie or that new girl at the clinic who is almost always wearing a scarf. I am a fourth year student from the University of Alberta currently finishing my undergraduate degree in Kinesiology. As part of my degree program, I have the wonderful opportunity of being placed in Fort Saskatchewan for a 14-week practicum to learn from and observe the knowledgeable staff and physiotherapists.
Through my series of blogs, my intention is not only to learn about specific health conditions, but to also pass along the information I have gathered from my academic research.
MYASTHENIA GRAVIS
In my first few days of placement at Pivotal Physiotherapy, I was introduced to a patient with Myasthenia Gravis. What is Myasthenia Gravis you may ask? Well I was asking the very same question. I was very intrigued. After doing a little bit of research, I began to understand the condition more clearly. I figured I’d share my findings with you and discuss how a condition like Myasthenia Gravis impacts an individual’s life and how it can be managed in a physiotherapy setting.
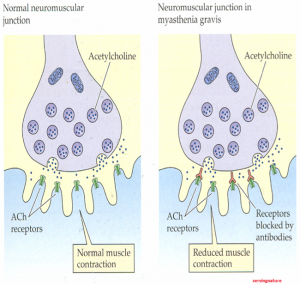
For starters, Myasthenia Gravis (MG) is a progressive autoimmune disease in which the body produces antibodies which attack receptors on the muscles surface. 4 These receptors are known as acetylcholine receptors (AChR). Acetylcholine is a chemical released from nerves that binds like a puzzle piece onto receptor sites on the muscle. This binding triggers muscle contraction. However, when antibodies attack these receptors they fill the space which acetylcholine would normally attach to and leave very few sites for acetylcholine to bind. 4, 5 The result is very poor binding of acetylcholine onto muscles receptors; since acetylcholine is required for muscle contraction, this will cause weak muscle contraction. 2
Figure 1.
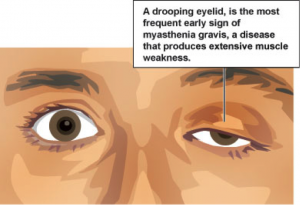
Research has shown that muscle weakness is worsened with the continued use of muscles.4 Many of the muscles within our bodies are constantly at work: all the muscles that help us maintain our posture and perform daily functions, also the muscles of our eyes, mouth, and lungs. Therefore, it is not surprising that symptoms of MG would display: 1, 2, 4, 5, 7
– General muscle weakness & fatigability
– Drooping eye lids
– Difficulty breathing
– Difficulty with chewing & swallowing
– Difficulty talking
EXERCISE – GOOD OR BAD?
A common belief is that exercise is a poor choice for individuals with MG. Since we know that repeated use of muscles causes muscle weakness, it may be perceived that exercise will only bring on more weakness or fatigue, exacerbating the condition.
Figure 3.
Very few studies have been conducted on the impact of exercise on MG; as a result, additional studies need to be conducted to further understand this relationship. However, as of now, studies have shown that “carefully prescribed and structured exercise programs can improve aerobic exercise capacity and muscle strength.” 5
We know that exercise is of importance to keep bones and muscles strong to help maintain ones mobility in the general population, so why should this not apply to individuals with MG?
Low impact exercises such as walking, swimming, and light jogging may actually reduce fatigue in patients with MG. In general, the reason why exercise exasperates symptoms in individuals with MG is due to pre-existing inactivity. A condition such as MG often motivates individuals to engage in more sedentary behavior for fear of worsening symptoms with exercise. Once sedentary, muscles become weakened and any degree of exercise will place stress on muscles and hasten fatigue.
Inactivity can hasten the development of secondary health conditions such as, 7 Obesity, Coronary heart disease, Muscular Weakness and Osteoporosis or low bone mineral density.
Keeping the body active is a great strategy to maintain mobility and muscle function, but also to prevent secondary complications associated with sedentary behavior. For most people, regular exercise leads to increased muscular strength, endurance, and improved cardiorespiratory health– the same is true for individuals with MG.5 While exercise can’t reverse the body’s autoimmune response to acetylcholine receptors, it will keep the body strong and reduce the chances of developing secondary health conditions which complicate MG symptoms.
Figure 4.
Figure 5.
On the contrary, participating in competitive sports or engaging in ultra-endurance events is not suggested for individuals with MG. One reported case of an ultra-marathoner with MG, revealed that even while on heavy doses of medication to control his symptoms, the strain of running 220 km race caused muscular cramps and weakness, difficulty swallowing and breathing.
EXERCISE CONSIDERATIONS FOR INDIVIDUALS WITH MYASTHENIA GRAVIS
When engaging in exercise, individuals with MG must be cautious. They must consider the time of day in which they exercise, type of exercise, duration of exercise, and the environment in which they exercise.
Because fatigue is a common symptom of MG, individuals with this condition should exercise in the morning when they have the most energy and are least fatigued, since muscular weakness is usually heightened in the evening. 4 Being conscious of timing to avoid fatigue not only applies to exercise, but also to the eating schedules of individuals with MG. Chewing is essentially an exercise which works the muscles of the jaw. If these muscles experience too much fatigue, individuals may be at greater risk of choking because their food is inadequately chewed. To combat this, meals should also be planned with the largest meals of the day coinciding with the time at which the individual is least fatigued.
Figure 6.
Additionally, “Excessive heat can bring on muscle weakness as well as other MG symptoms.” 6 As a result, exercise sessions are best limited to the mornings when temperatures are lower, or performed in indoor facilities to avoid hot, humid outdoor environments.
To ensure safety while exercising, PACE is a suitable guideline to follow. 8
P- Planning daily activities
A- Adapting the home, adequate rest, assistive equipment, asking for help
C- Conserving energy, check-ups with doctor, cool temperature
E- Emotional stability, exercising in moderation, eliminating unnecessary daily tasks
EXERCISE PRESCRIPTION
Although there are no set guidelines for exercise intensity, duration and load for individuals with MG, regular to moderate exercise in the form of walking swimming, jogging or recreational sports can combat muscle weakness. 6 Exercise should be repeated, yet only performed at a level which falls short of muscular fatigue. 6
In a physiotherapy clinic, exercise progression should be based on the needs of each individual. Some cases of MG are less progressive, meaning individuals may be able to tolerate more exercise, while in other circumstances, less exercise may be advisable.
All strengthening exercises should progress first from range of motion exercises to emphasize flexibility to exercises using light resistance in the form of a thera-band and finally to full resistance exercises using machines and free weights. A general exercise prescription for an average individual is 3 sets of 10 repetitions, while no distinct guidelines exist for individuals with MG, starting with a lower prescription of 3 sets of 5 repetitions may be advisable.
Nicole Geier BScKin Student
References
References 1 Cass, S. (2013). Myasthenia Gravis and Sports Participation. ACSM Current Sports medicine
Reports, 12(1). 18-21.
2 Davidson, L., Hale, L., & Mulligan, H. (2005). Exercise prescription in the physiotherapeutic management of Myasthenia Gravis: a case report. NZ Journal of Physiotherapy, 33(1). 13-18.
3 Elsais, A., Johansen, B., & Kerty, E. (2010). Airway limitation and exercise intolerance in well-regulated myasthenia gravis patients. Acta Neurol Scand, 122(190). 12–17.
4 Nastuk, M.A. (2013). Myasthenia gravis. Magill’s Medical Guide, (Online Edition). 5 Scheer, B.V., Valero-Burgos, E., & Costa, R. (2012). Myasthenia gravis and endurance exercise. Am. J. Phys. Med. Rehabil., 91(8). 725-727. 6 Myasthenia Gravis Association. (n.d.). Exercise, Heat, & Nutrition. Retrieved from:
http://mgakc.org/newly-diagnosed/exercise-nutrition
7 Myasthenia Gravis Foundation of America. (Fall, 2009). Foundation Focus. Retrieved from http://www.myasthenia.org/LinkClick.aspx?fileticket=IjjLgniJi1E%3D&tabid=75
8 PTC Physical Therapy. (n.d.). Exercise and myasthenia gravis.Retrieved from http:// www.my-physical-therapy-coach.com/exercise-and-myasthenia-gravis-mg.html
9 The Australian Myasthenic Association in NSW. (n.d.). Myasthenia Gravis. Retrieved from http://www.myasthenia.org.au/html/background.htm
Figure References
Figure 1. Retrieved from: http://1.bp.blogspot.com/-50wzSCJdY1Q/UUC7YGGzVtI/ AAAAAAAAAhE/BpvYmzUV4Y4/s1600/NMJ+-servingnature.png
Figure 2. Retrieved from: http://www.nation.lk/2010/05/09/ey4.jpg
Figure 3. Retrieved from: https://s-media-cache-ak0.pinimg.com/236x/48/9d/ d3/489dd3ea8fc492e98f18813a8e915d0b.jpg
Figure 4. Retrieved from: http://www.satvikshop.com/blog/wp-content/uploads/2013/02/ walk4health.jpg
Figure 5. Retrieved from: http://www.cscitech.com/wp-content/uploads/2015/02/JOG-2.jpg
Figure 6. Retrieved from: http://eattobeatmyastheniagravis.com/wp-content/uploads/2014/03/ natural-excercise.jpg